My ResMed AirSense 10 AutoSet trial arrived a couple of weeks ago. After setting it up and picking some starting options the data flowed for roughly two weeks. Nasal pillows are not suitable for me. They cause my mouth to open creating the strangest air pressure sensations. The ResMed N20 full face mask it is! 😷
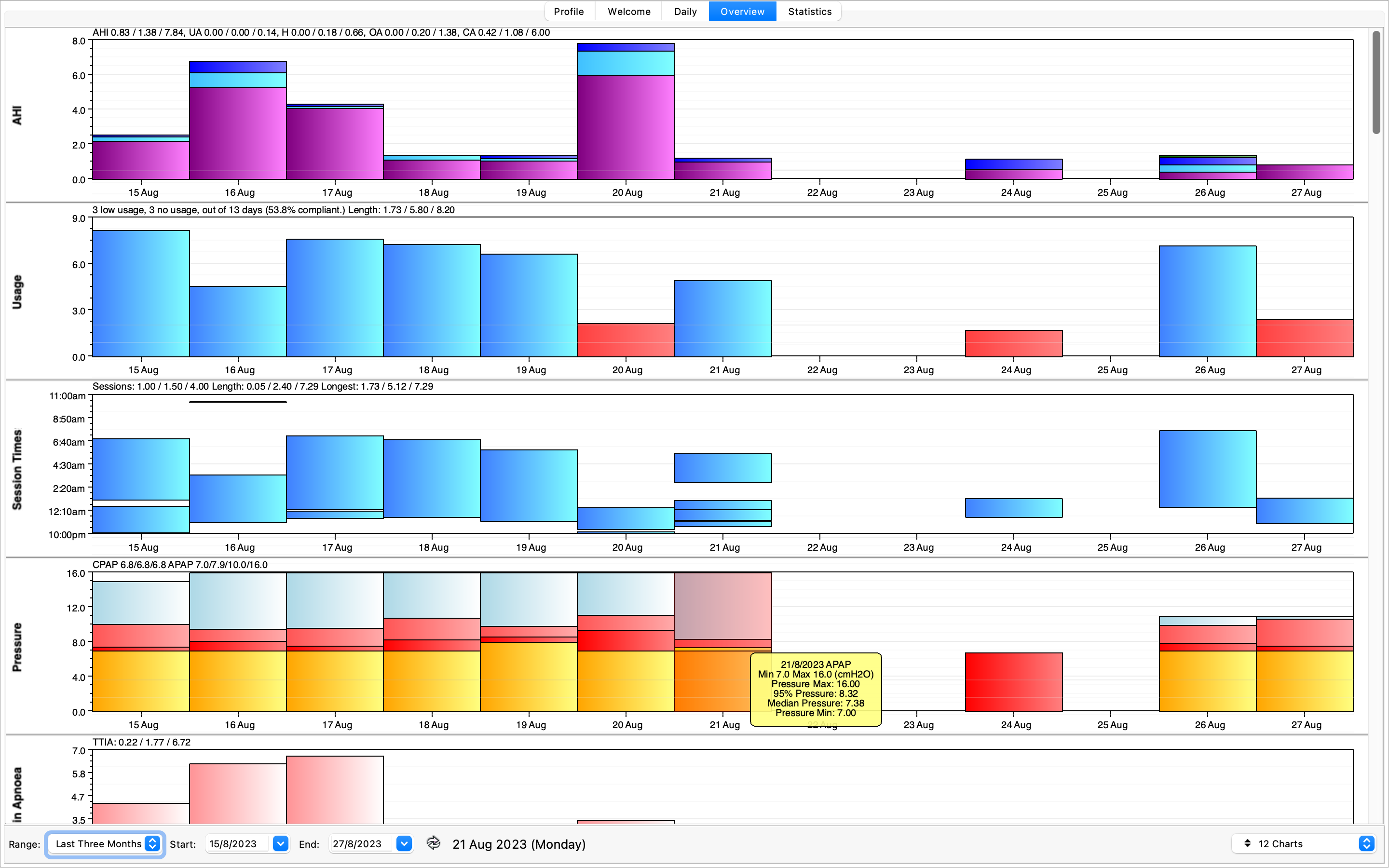
Using the Open Source CPAP Analysis Reporter (OSCAR v1.4.0), we can delve a into the data. Any days missing data are due to insomnia keeping me awake all night. I’ve put the data into a zip file here too. Not fun. Anyway, let’s look at some of the days in more detail and the different event types.
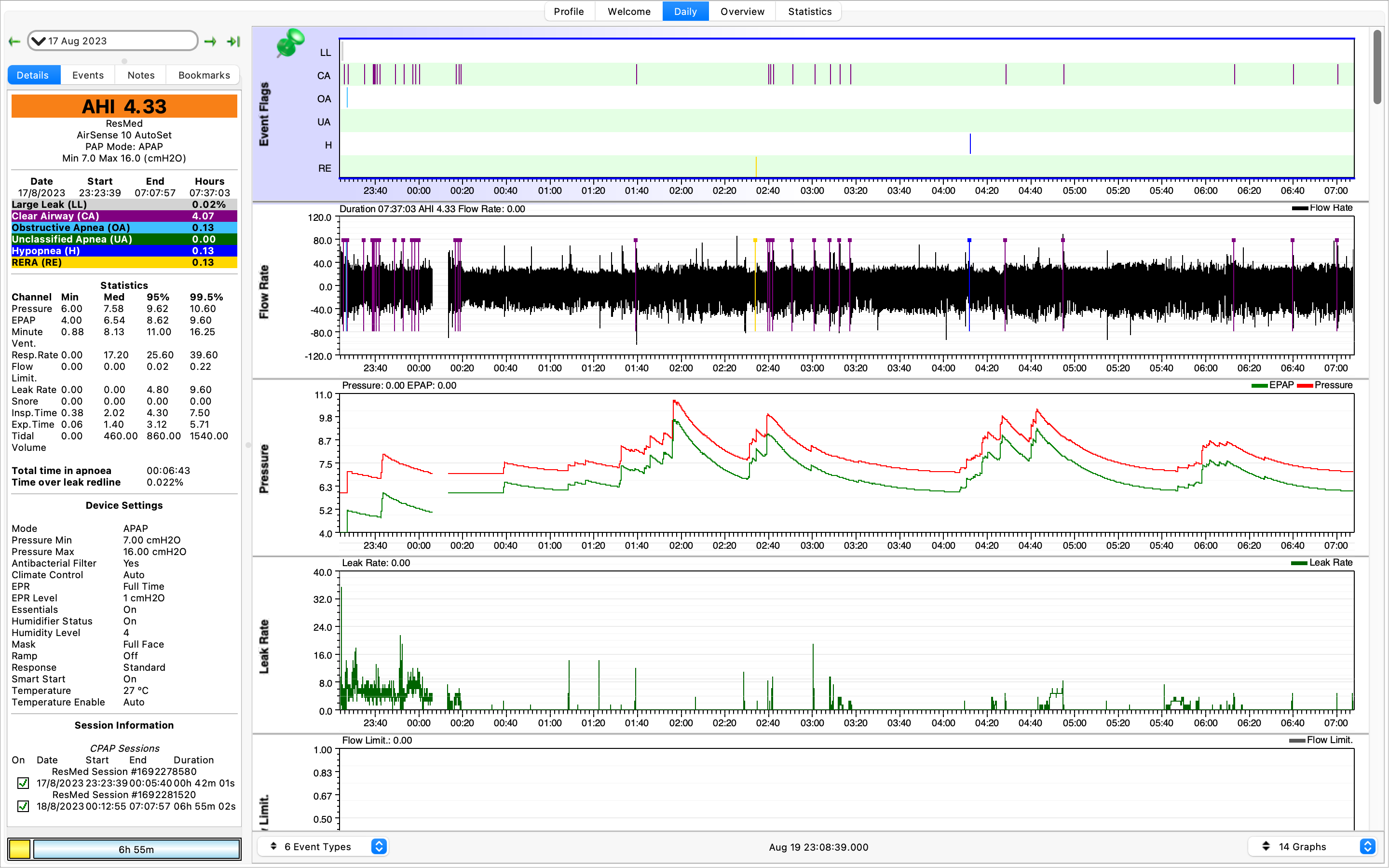
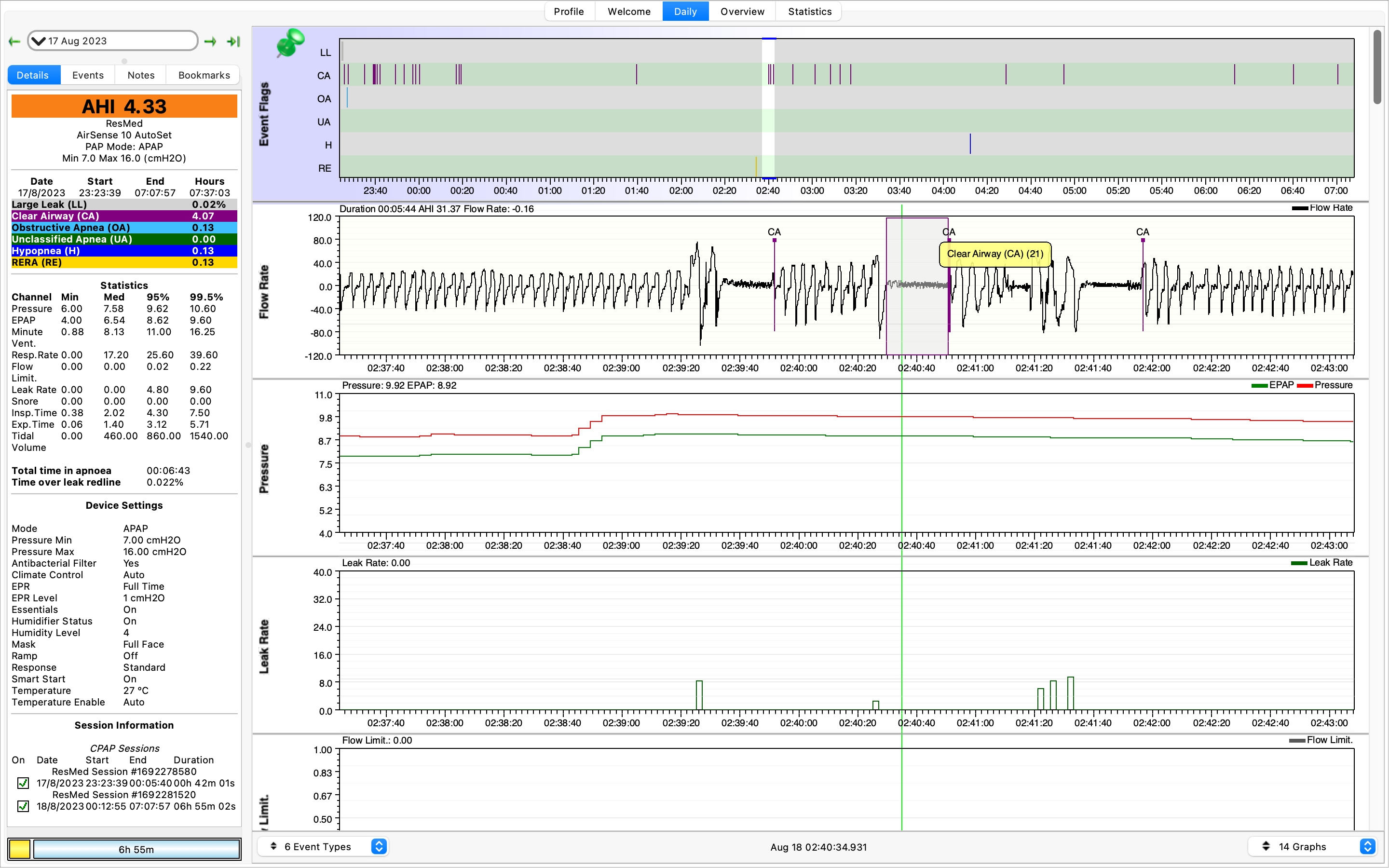
We’ll start off with longer periods of recorded data. Above is the 17th August. Many nights were only a few hours of data because the mask itself would cause me to wake up. A lot of clear airway or central apnea events (CAs). If we disregard the earlier data in the night while I was trying to begin sleeping, we can see some of these CA events.
21 seconds, without breathing. Interesting. While awake I tend to be a shallow breather. So not breathing during sleep would not surprise me in the slightest.
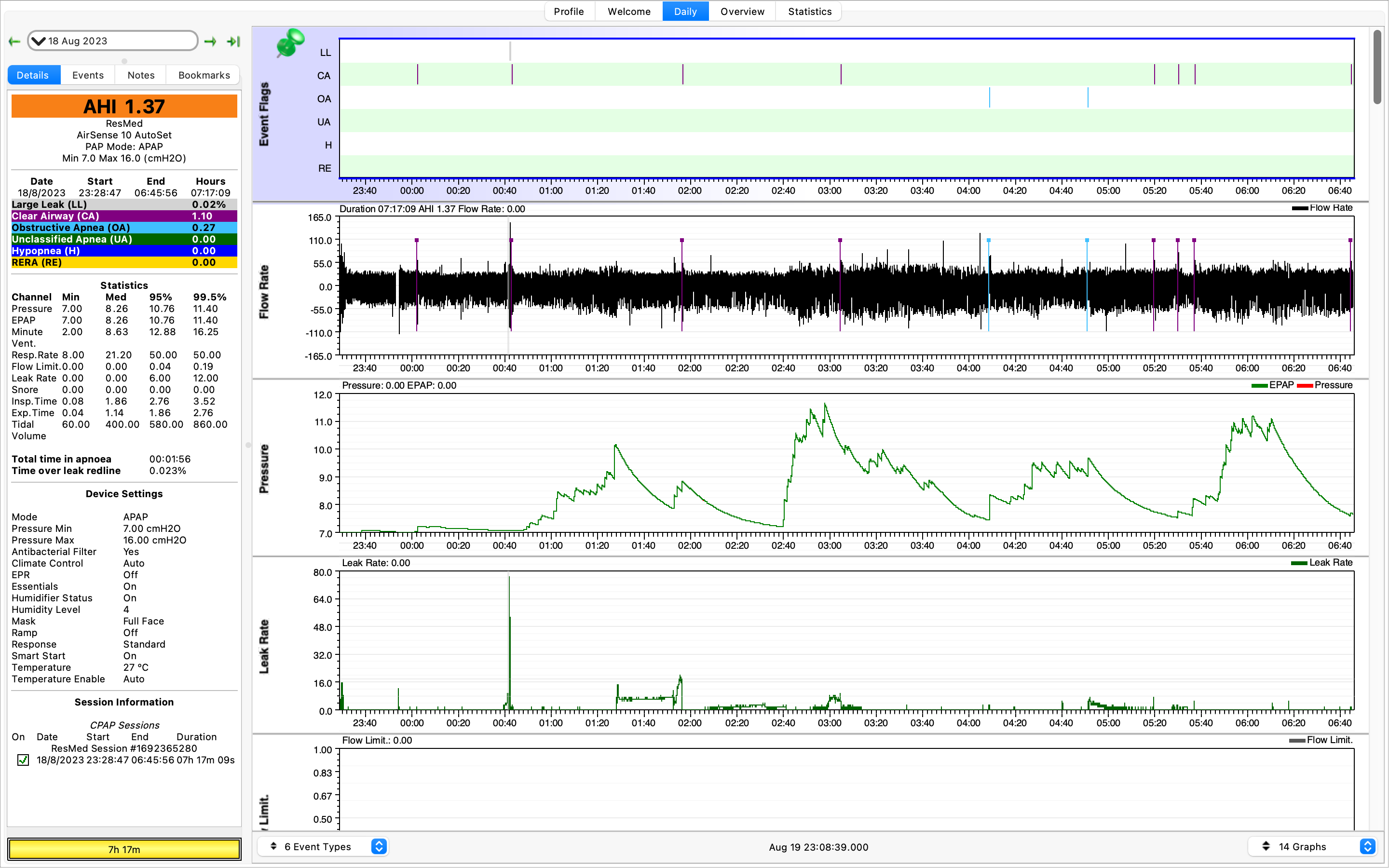
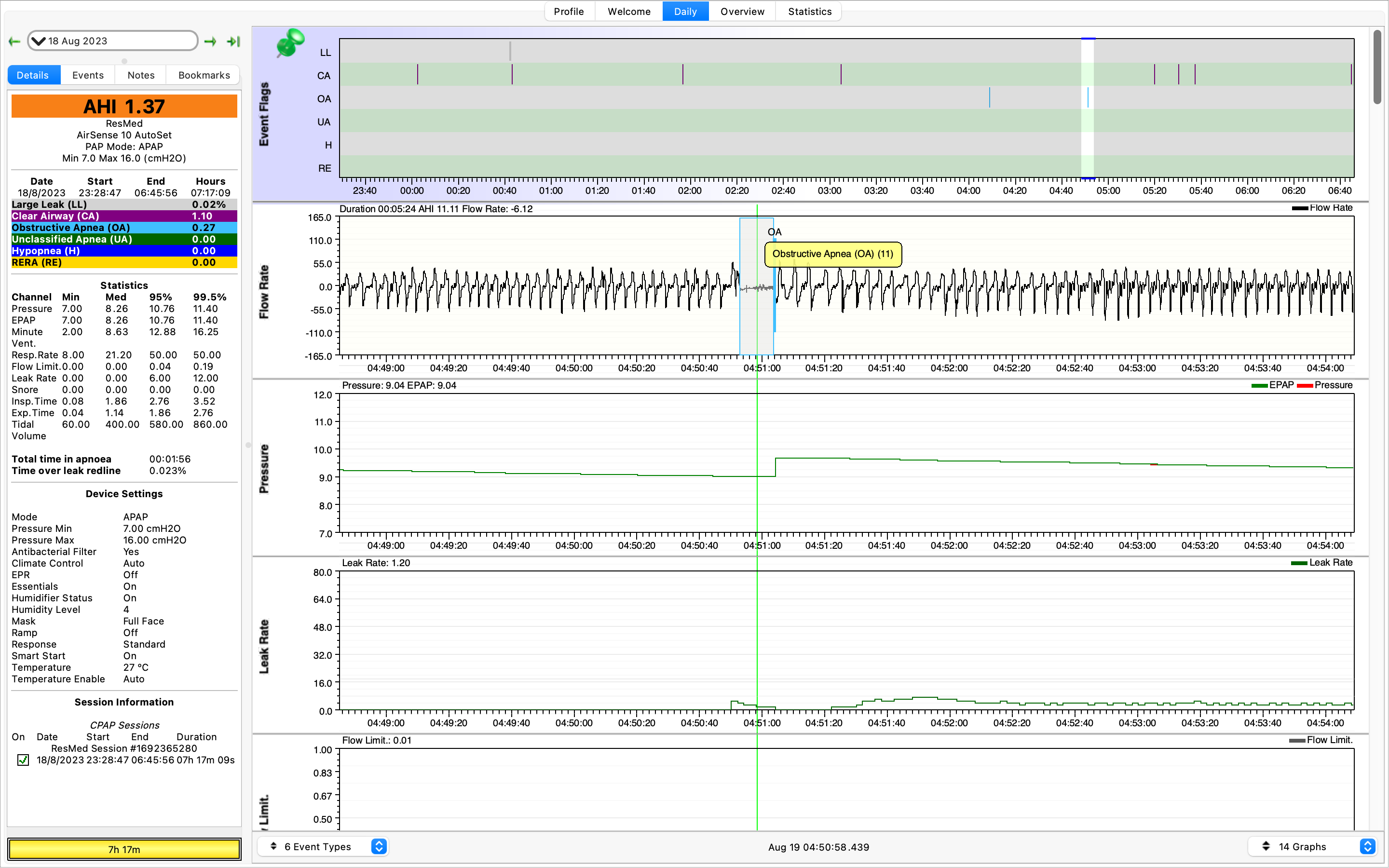
Here’s the 18th August, and we have recorded some obstructive apneas (OAs).
How does the software distinguish between CA and OA though? On the above, I couldn’t see any data in the many graphs that would tell them apart. What’s also interesting is that resolving OAs can result in treatment-emergent central sleep apnea…
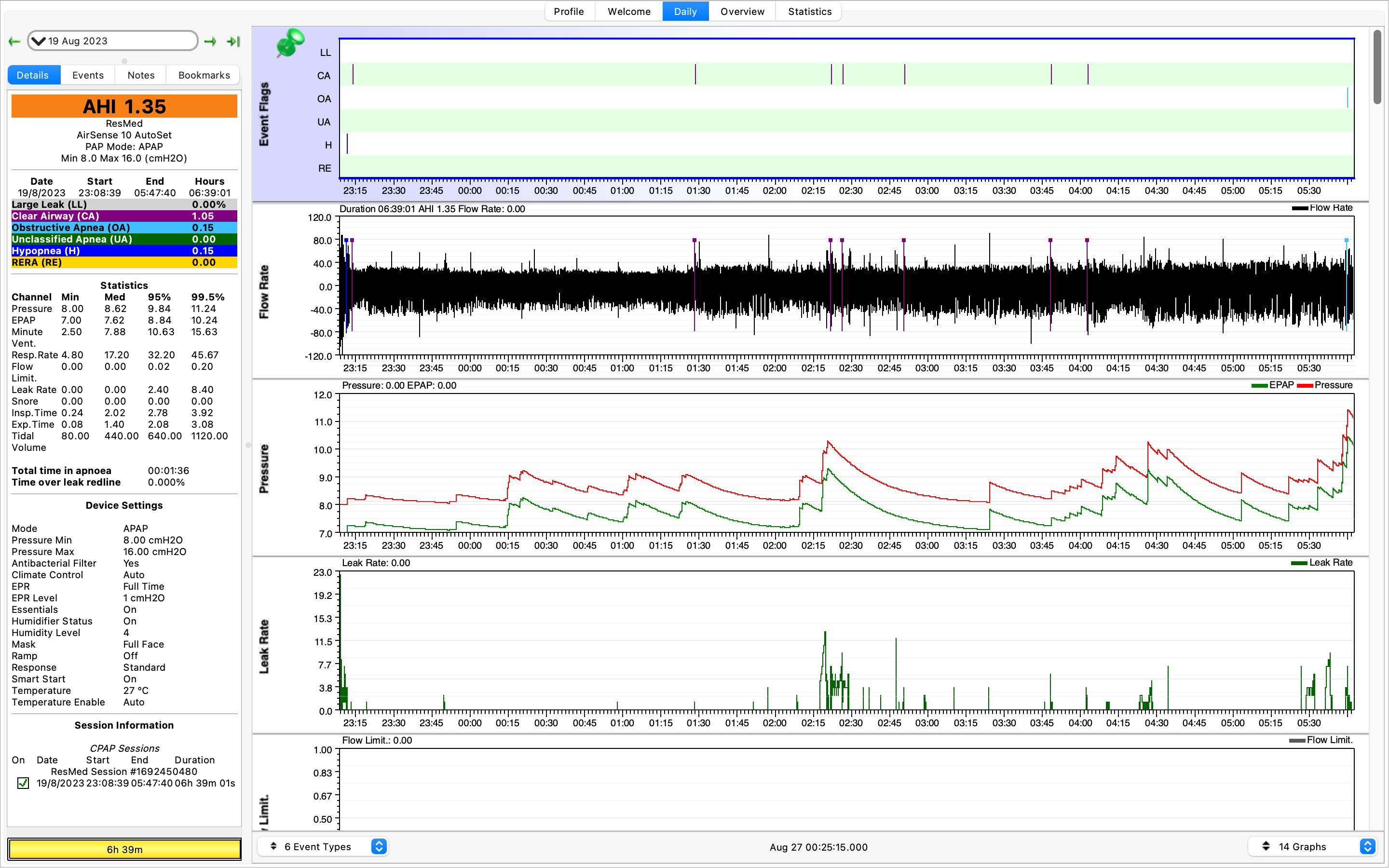
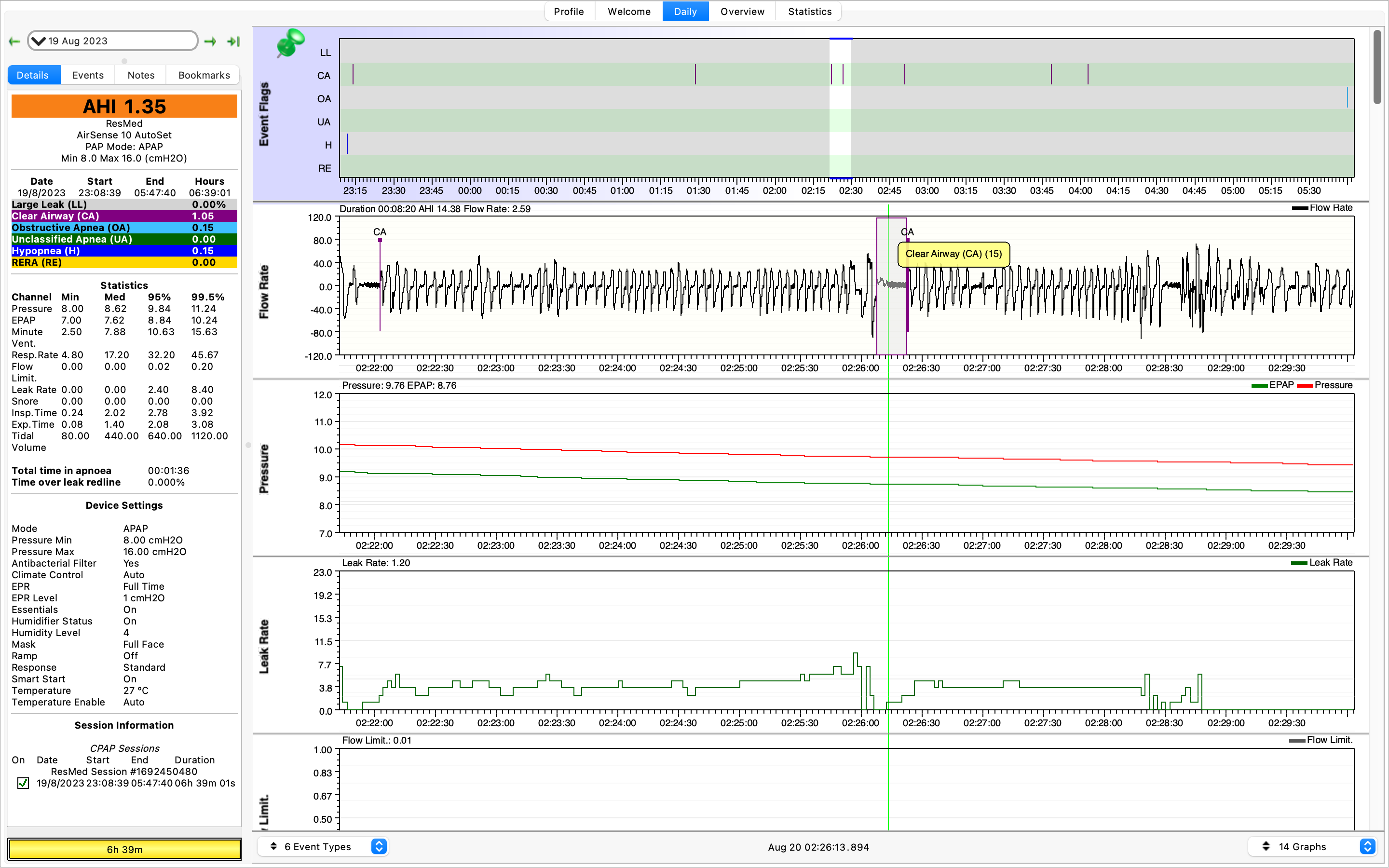
Here’s some data from the 19th August. Keeping the AHI below five is apparently something people like to do. My AHI was below five on most days and never exceeded eight.
A few more CA events. If they are around 10 seconds they aren’t usually a cause for concern. The 20+ second ones above are probably of more concern.
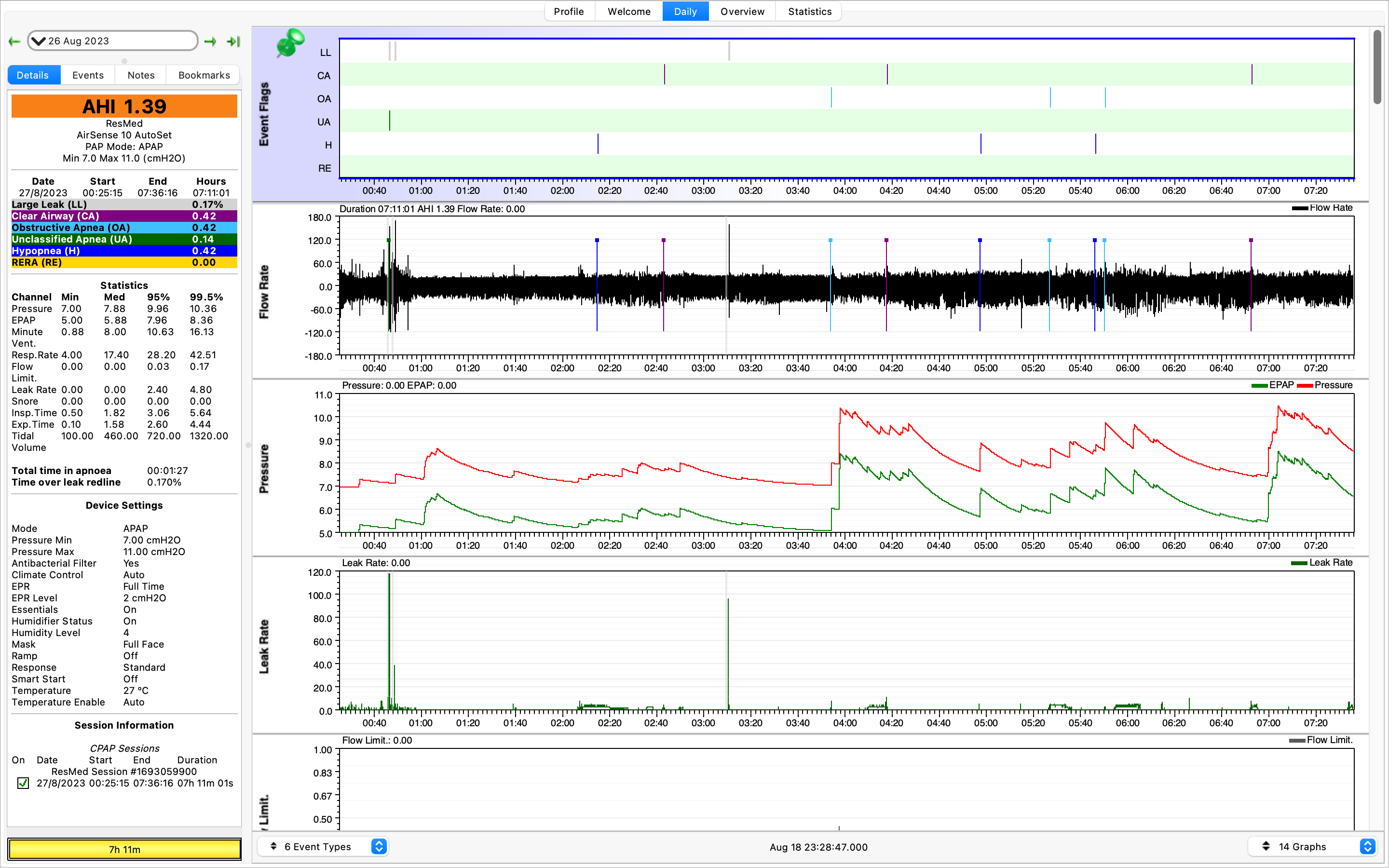
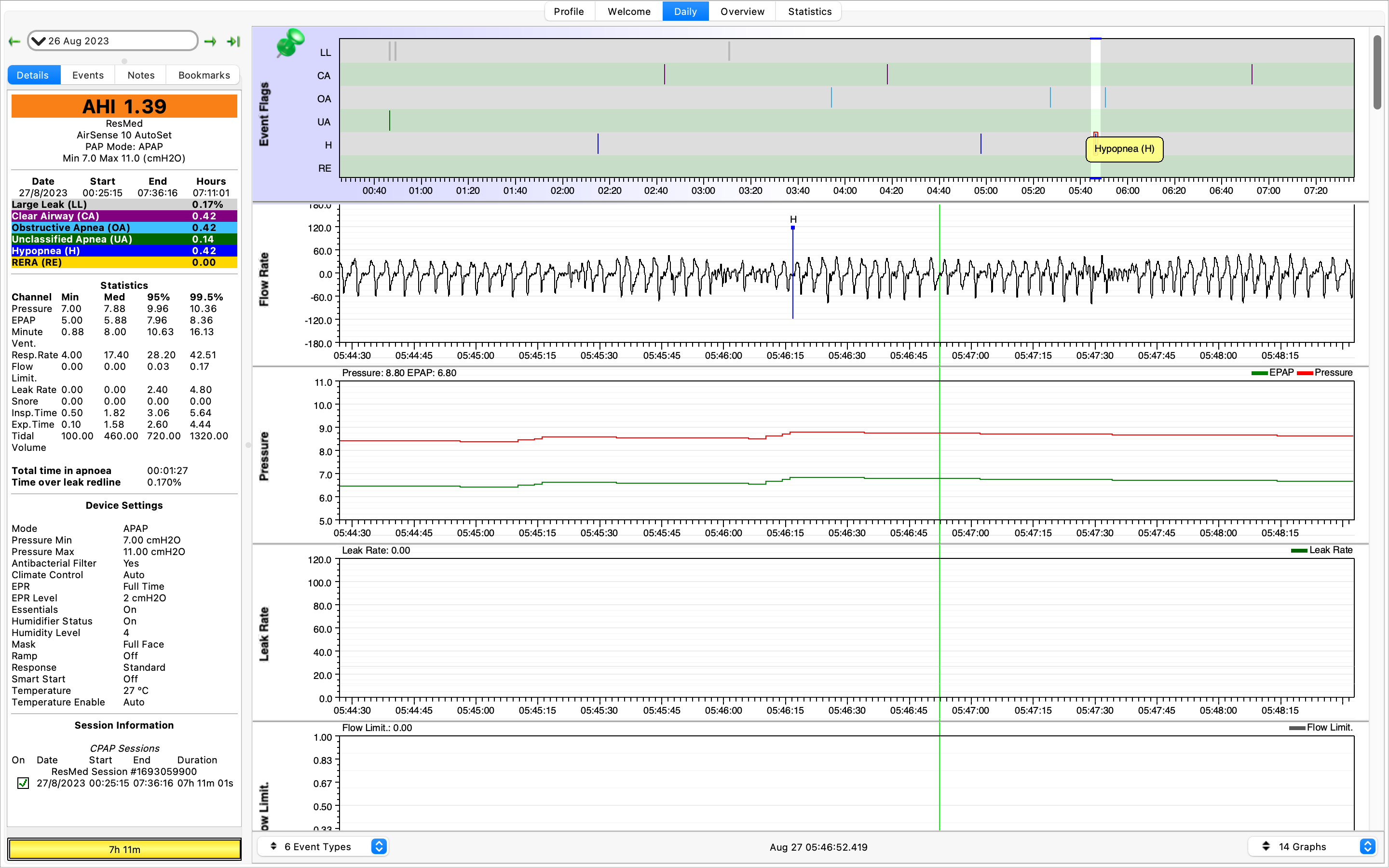
Jumping forward a week to the 26th August we have more data. This one has it all! Large leaks (LL), CAs, OAs, and hypopneas (H). Large leaks are usually caused by readjusting the mask.
There’s a hypopnea (hypo=under, pnea=to breathe). Makes sense, not as flow rate decreased from the machine to the mask.
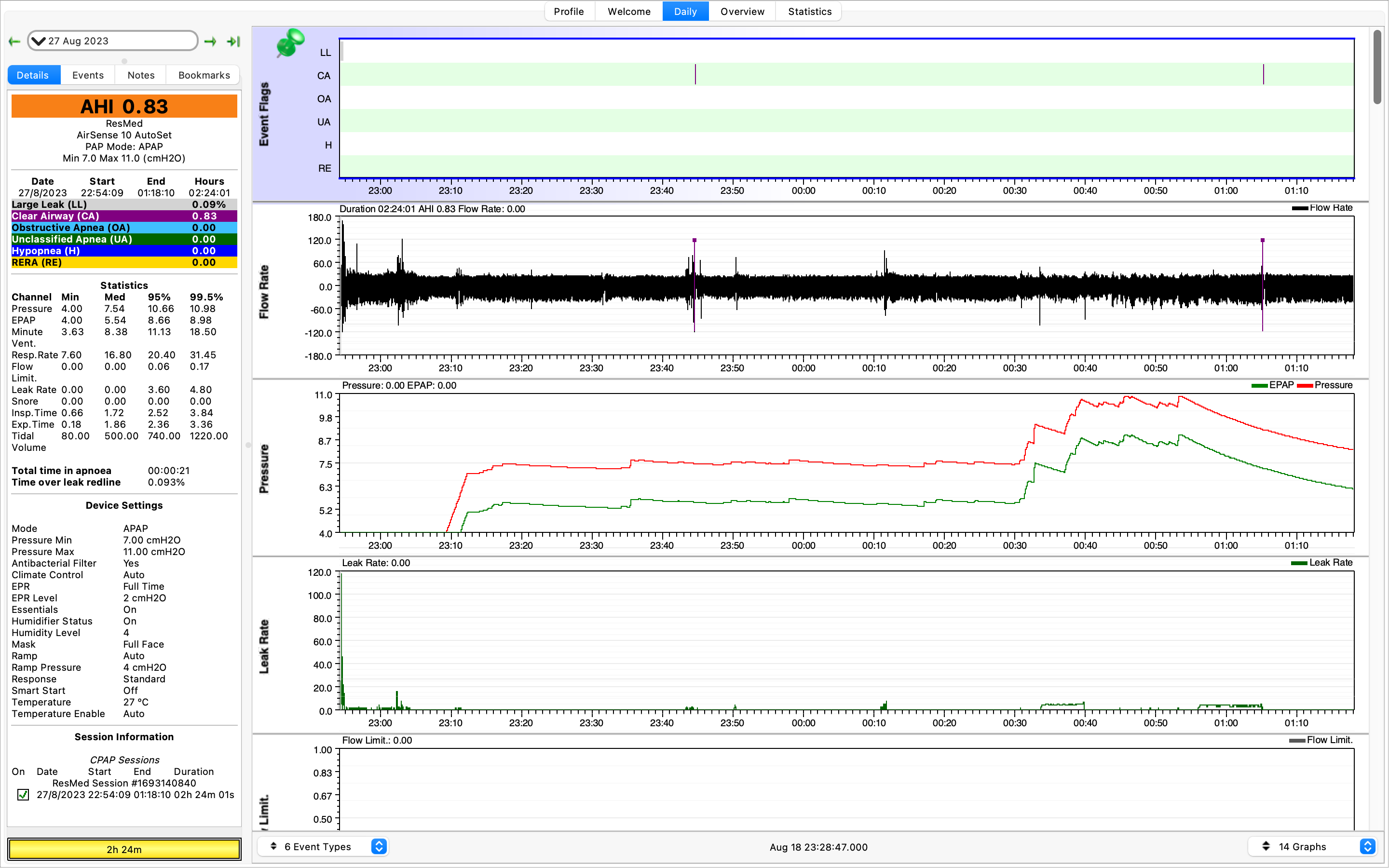
And the last day of recorded data where the pressure ramped up to 11 and I threw the mask off after a few hours.
What have I learnt from this. While my snoring might be an issue to any roommates it does not affect me day-to-day. I varied the settings on the machine night to night but found that adjusting EPAP, to allow the pressure to drop while exhaling, made it much easier to sleep.
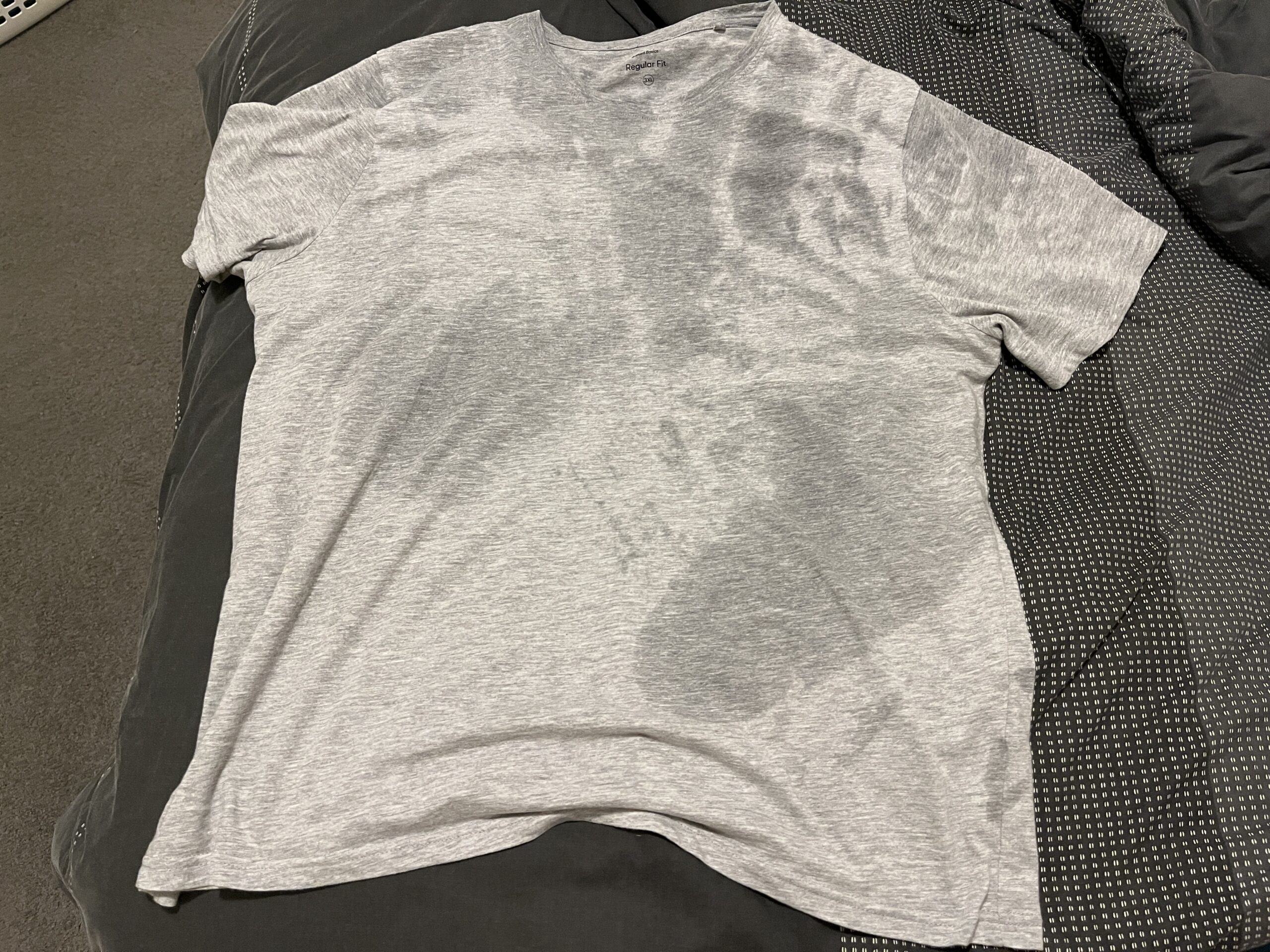
However, I did not feel more rested. What’s worse is there were at least three days where I woke up sweat drenched. This was one of the things I was trying to solve – night sweats. I suppose it isn’t because I snore and stop breathing during sleep.
Will APAP or CPAP solve night sweats? For me, no. And that was the primary question I wanted answered. I still have a sleep study in the future. However the inconsistent frequency of night sweats ~20% of nights (3 days in 14 days) does not bode well for being detected on one night of sleep testing.
I guess all I can do is continue to have issues getting to sleep and staying asleep. I’ve tried eliminating caffeine, reducing room temperature, sleeping positions, nothing seems to work. Coupled with phantom itches as I’m trying to sleep certainly doesn’t help either.
If not a physical issue, it’s going to be a psychological. Perhaps a simple combination of stress and anxiety running unchecked while I try to rest. 😮💨