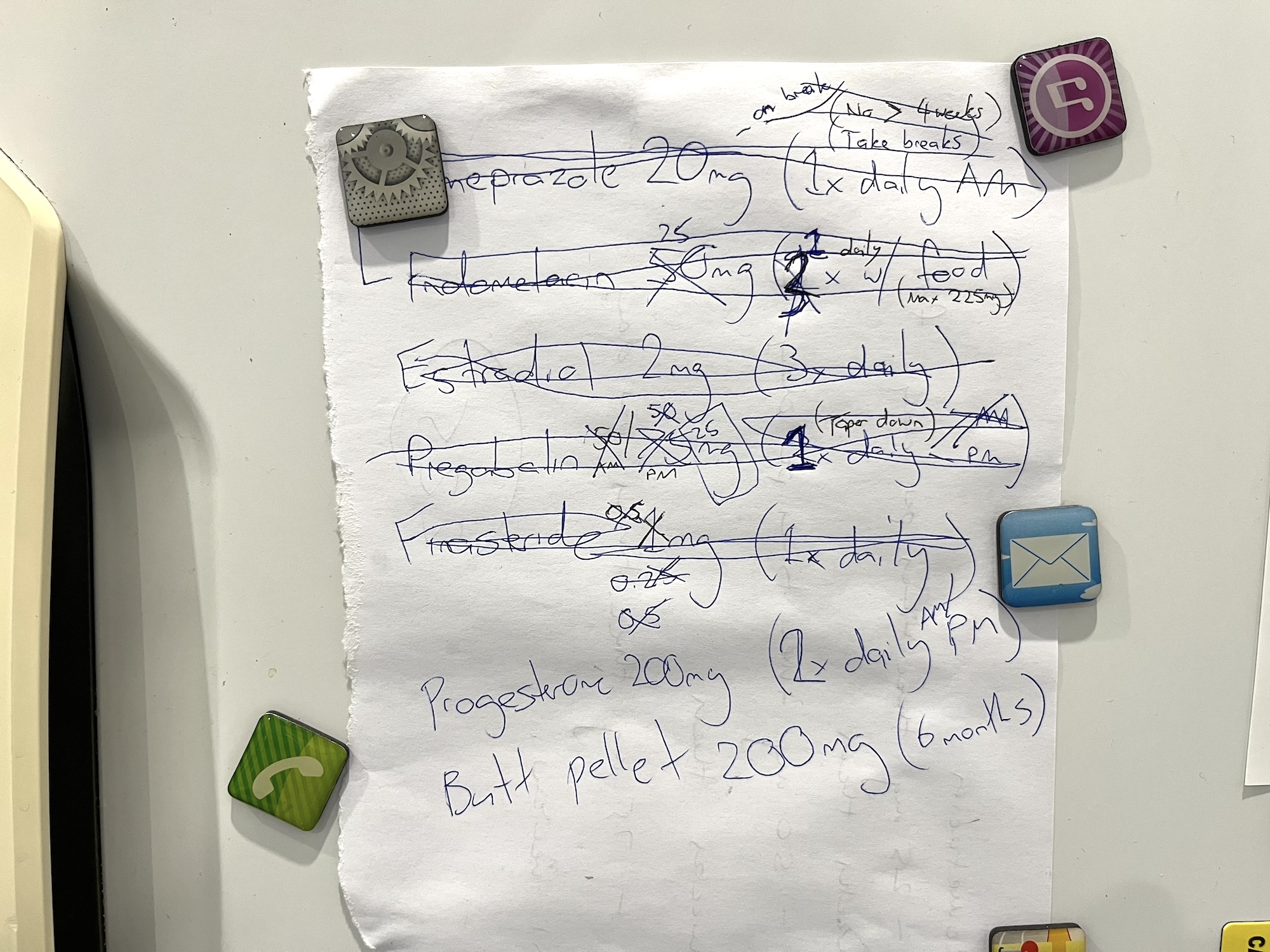
A few milestones have been achieved this month. I’ve reached my third month of gender affirming hormone therapy (GAHT) and was able to get an estradiol implant (200mg, compounded). I kicked pregabalin as it wasn’t helping with my anxiety symptoms – but was helping with sleep… I also ceased indometacin successfully. Hemicrania continua is not being so continua now.
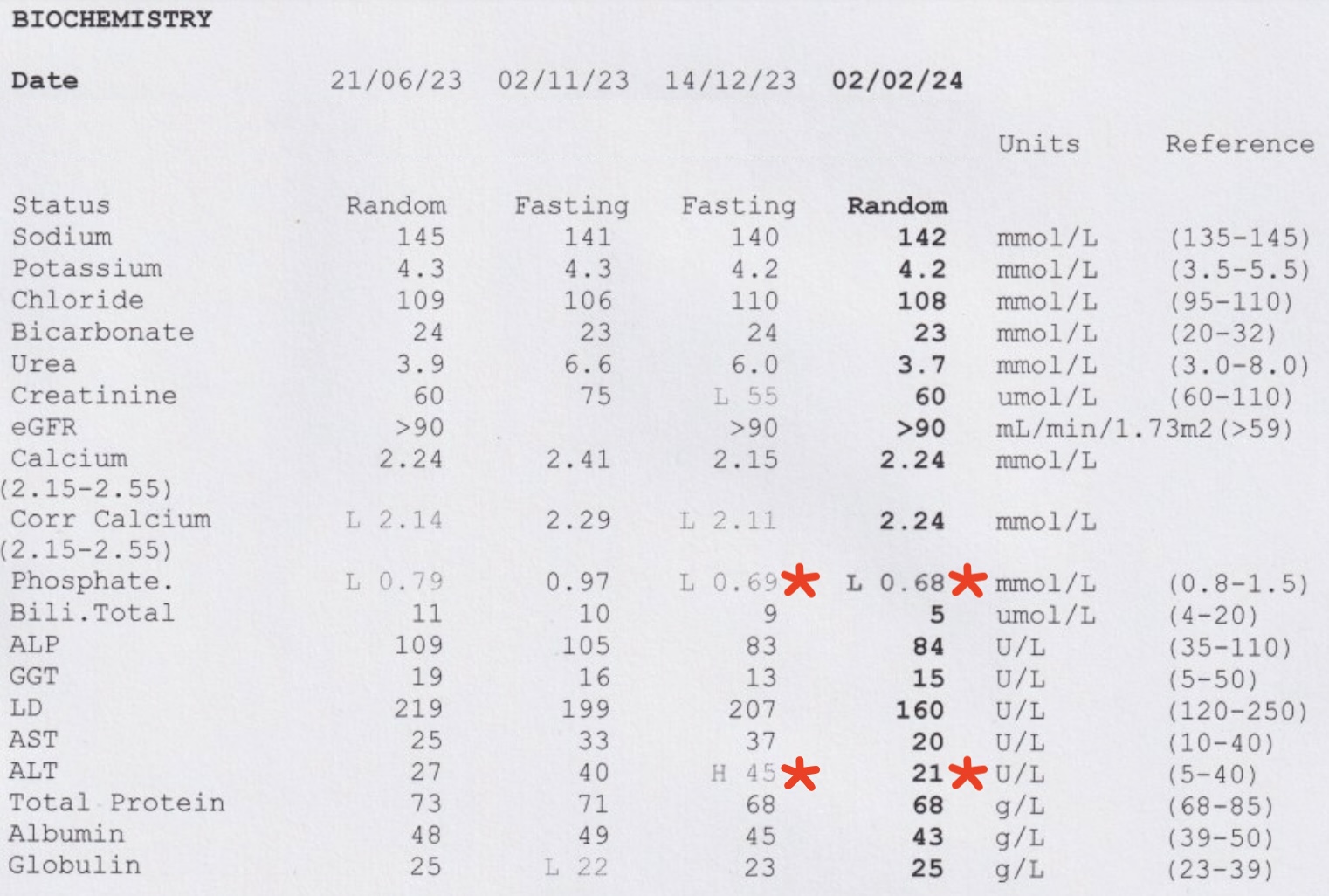
My phosphates, calcium and ALT levels. Ahhh yes. Let’s start with the ALT. My ALT was easy to fix, cease indometacin. I also took some milk thistle to help keep the old liver in tip top shape – with interesting consequences. I’ll circle back to this one later!
Phosphates and calcium, I do wonder if this is actually a bad thing to have lower numbers on these. A ionised calcium test was ordered and found to be in range, but so were my other calcium stats – this time. I’d only changed my calcium vitamin to a non-plant-based formula as I don’t get much calcium from milk. i.e. I don’t drink milk. End result – calcium levels are OK for now.
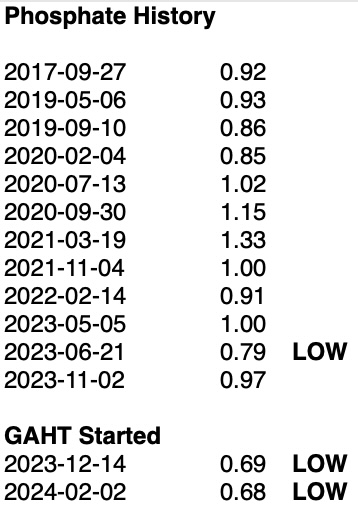
Now phosphates are in everything, it should be difficult to ingest this in low amounts. Thankfully, I have a good history owing to low blood iron and phosphate levels were ordered as a complementary test most of the time. Using this data we can see that I tend to be on the lower side of things. But since starting GAHT, record new lows. Some potential answers could be here and here.
My theory is either my spirulina (cyanobacteria) infused multivitamin is causing lowered calcium and phosphate levels leading to improved bone density. This could perhaps explain the historically lower phosphate levels as I’ve taken this particular multivitamin for a few years now. Then we have this (potato) gem from the second article.
Estrogen therapy (ET) is associated with lower serum calcium and phosphorus concentrations and is known to increase bone mineral density (BMD).
Estrogen and progesterone are very good at not causing osteoporosis. Menopause is a great example of what happens when hormones are absent and why hormone replacement therapy exists for older assigned female at birth (AFAB) people. This puts my mind at ease and we’ll be rechecking in three months.
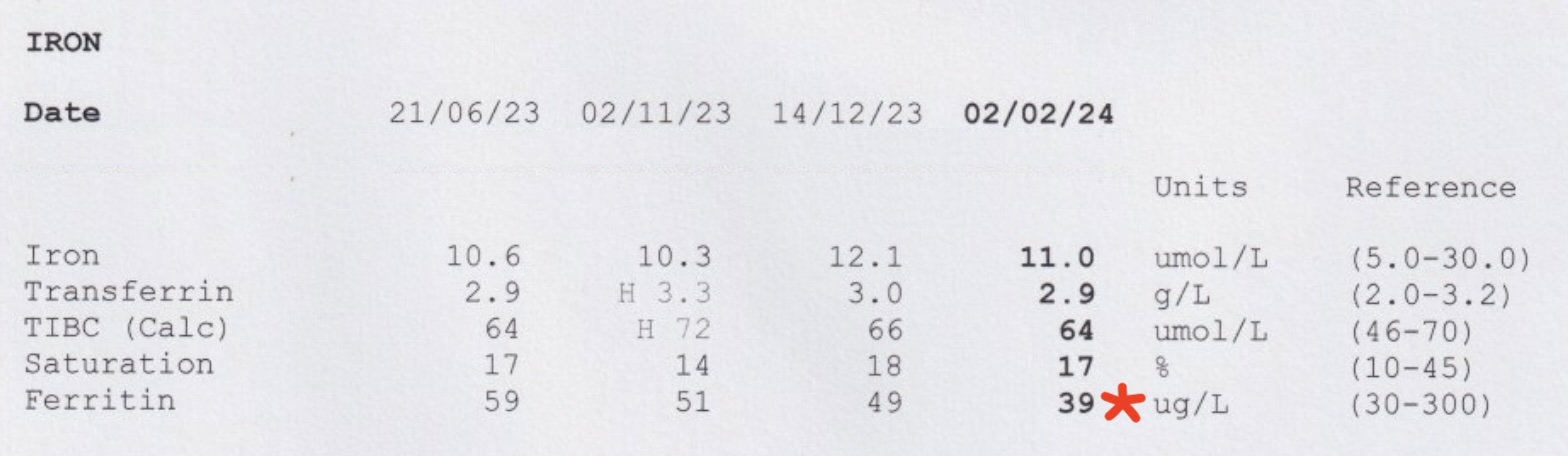
Oh iron, sweet, sweet iron. I mean each blood test takes five vials of blood? I’ve given up on blood donations so we can rule that one out and it’s nothing cancer-related so… diet? To keep my ferritin (iron stores) up I’ll be taking 210 mg of elemental iron every other morning one hour before food. This maximises absorption as hepcidin, the enzyme that tells the iron to stay or go, is still sleepy.
Of course vitamin C can override this too if daily dosing was needed. As my levels haven’t reached critical yet, and I don’t enjoy the undesirable GI side effects of iron therapy, every other day gives me roughly half the issues! 😅
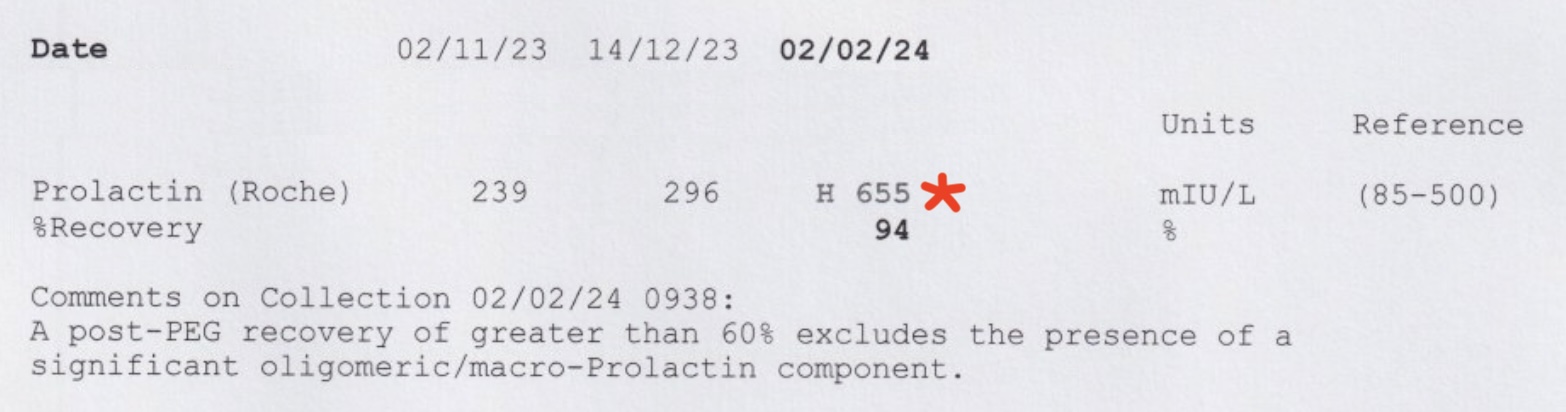
Onto hormones! Errrrr… why did prolactin double and zip outside the reference range in the space of two months. The GP wasn’t sure why and the endocrinologist said it’s not an issue unless it’s triple that number. I had a peek into some literature and pregnant women can have this level between 1000 and 8000 mIU/L. Remembering that pregnant women are not going to have those levels forever.
So what caused mine to spike? I believe it might have been the milk thistle I was taking to fix that pesky liver up from the indometacin damage. Information here, here and here. This has been ceased now so it should drop back within the reference range next blood test. Hold up, I was just reading this again.
In animals, milk thistle has been shown to stimulate bone mineralization. However, how it affects humans is currently unknown.
Hmmm, I wonder if my calcium and phosphate levels will also increase on next blood test without milk thistle supplementation. Something to look forward to as I was only on milk thistle for two weeks.
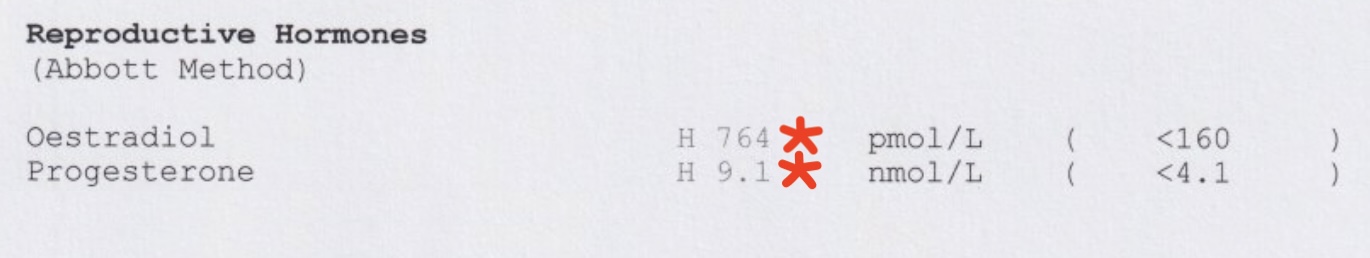
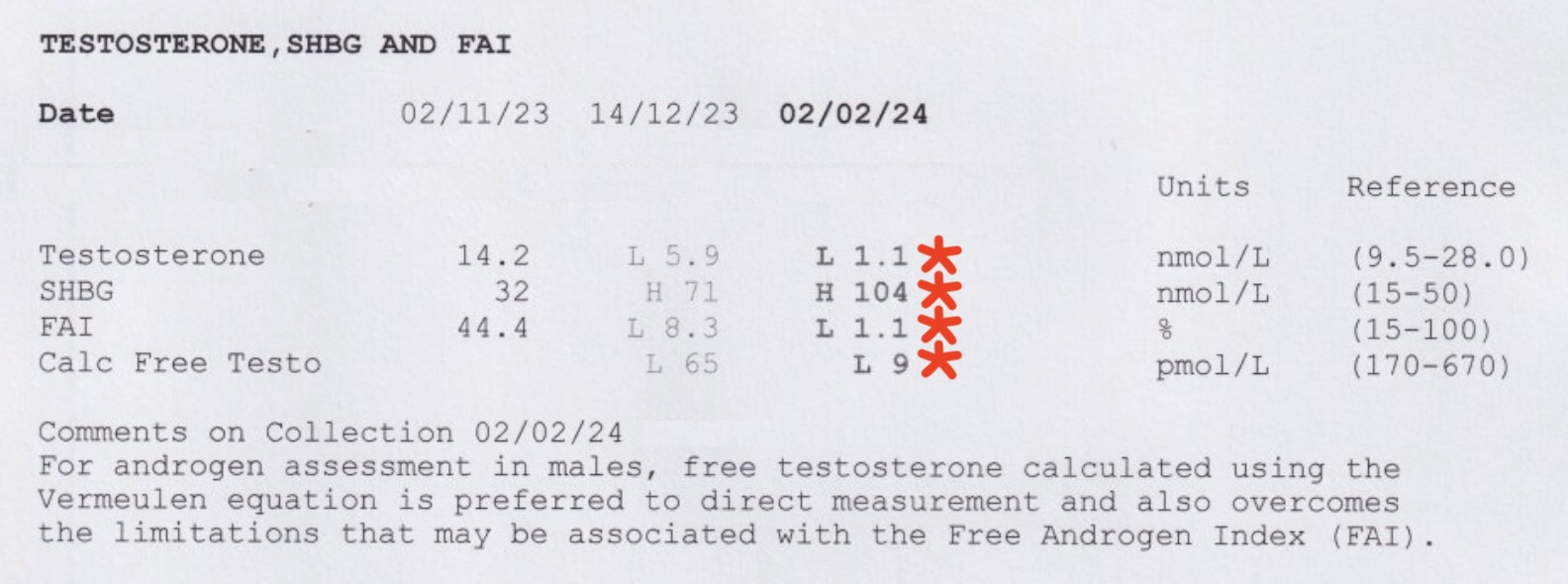
Ahh yes traditional sex hormones. One of the more interesting to look analyse. Keep in mind that all my blood tests are done in the trough – which should indicate the lowest concentrations.
On 6 mg oral estradiol valerate (2 mg thrice daily) and estradiol gel (Sandrena brand estradiol 0.1% gel 1g sachets twice daily) I scored a lovely 764 pmol/L. Previously with pill therapy (6 mg) it came in at 364 pmol/L. So a decent jump for just a bit of gel. Good result, so good in fact, I now I have two pellet implants (100mg each) in my left buttock for 200 mg of estradiol. It will be interesting to see how that stabilises over the next three months as they can fluctuate a bit early on.
On the progesterone (P4) front, folks tend to take it after being on estradiol for around 12 months. My endocrinologist doesn’t see any issue with starting it earlier. In AFAB puberty, estradiol peaks before progesterone even appears on the scene. Then again I am not exactly AFAB, so past performance may not be indicative of future performance.
For me, I see progesterone a counterweight against what is intended to be high-dose estrogen. With progesterone in the mix my skin is less dry which was one of my biggest gripes about estrogen monotherapy.
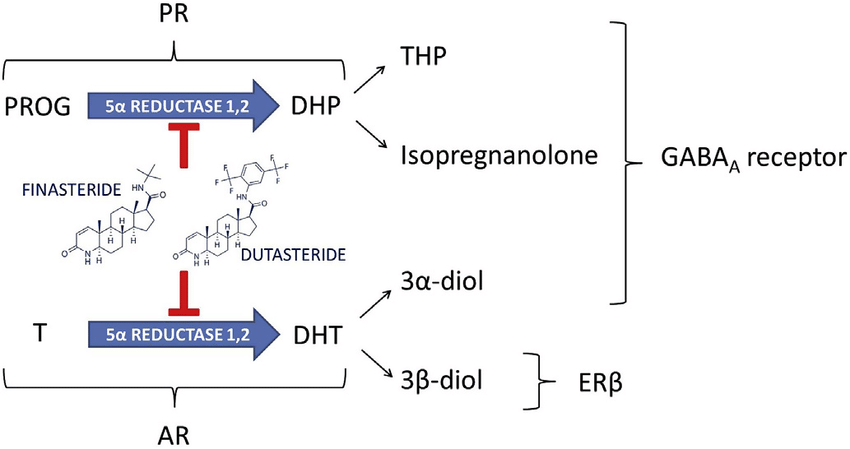
At least one of the metabolites produced, allopregnanolone, is a neurosteroid that acts on the GABAergic system when taken orally – in a good way, I think. Interestingly enough in a similar way to alcohol, benzodiazepines and even to a lesser degree, pregabalin. Lesser degree in that pregabalin doesn’t touch the GABA receptors themselves, and instead mess with other systems that have a flow on effect to the GABAergic system.
Oh I could ramble on for days about this sort of thing. Let’s look at the level itself. 9.1 nmol/L. Alright, that’s in the trough still so that’s quite good. Last dose would have been 12 hours ago. It puts me somewhere between pre-ovulation and mid-cycle. I have since doubled the dose on my endocrinologists recommendation.
There are other routes of administration (ROA) for progesterone, butt (ha!), my current compounded powder (200mg twice daily) is not compatible. I would need to purchase the non-compounded version to do that, and it’s not on my radar at this point in time as it is quite expensive.
Converting my 9.1 nmol/L to a US-friendly unit of 2.6 ng/mL helps locate where I am on these charts, you can see where I fit in. You’ll also maybe note that progesterone via the rectal ROA results in markedly different levels of progesterone, allopregnanolone and pregnanolone.
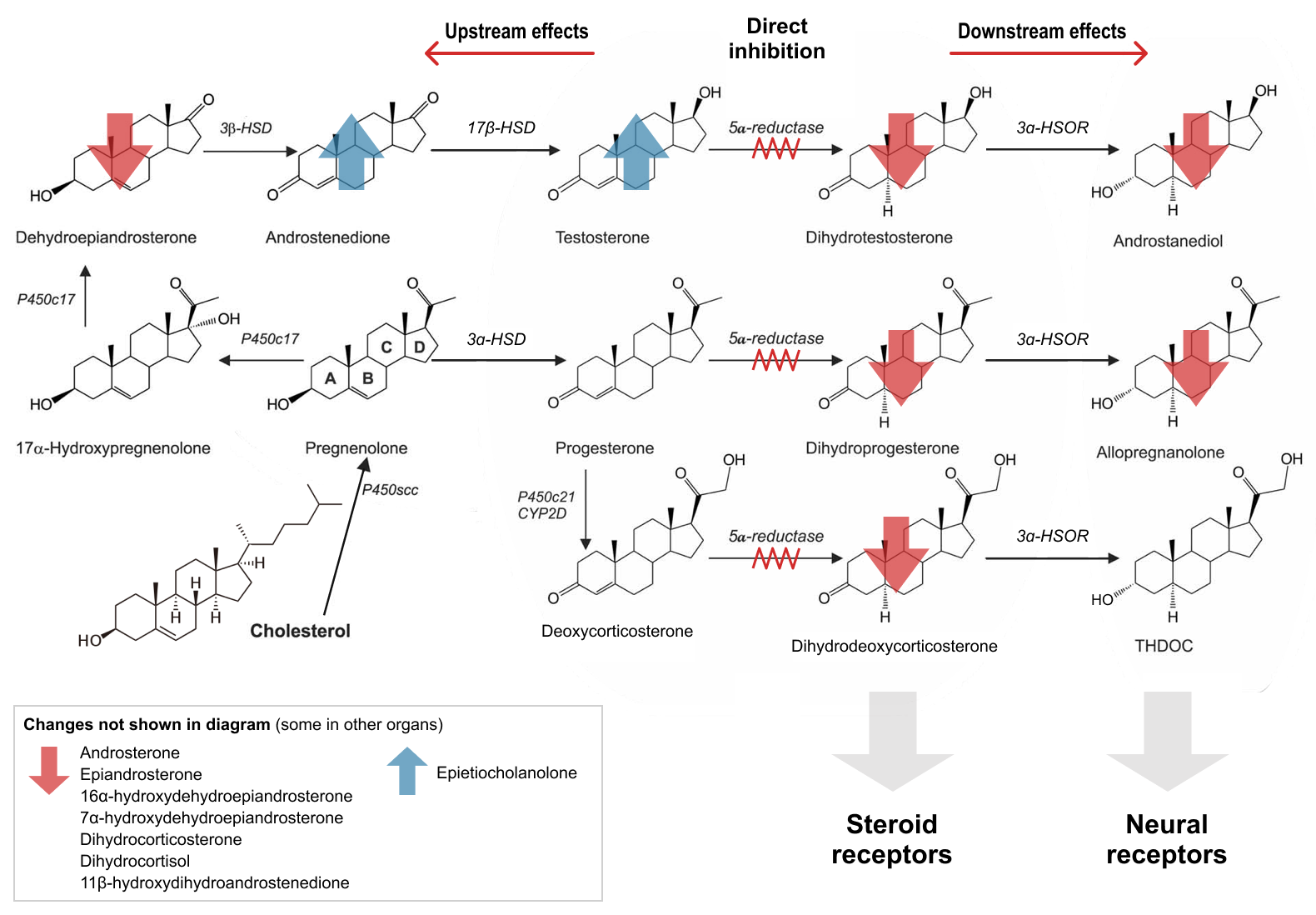
Which leads us onto finasteride which is a 5-alpha reductase inhibitor (5ARI). It stops this particular enzyme (5-alpha reductase) from doing what it wants to do. This is primarily used to stop testosterone (T) conversion to Dihydrotestosterone (DHT).
For assigned male at birth (AMAB) people, DHT gives you the gift of male pattern baldness provided you have the correct set of genes. As a transgender woman, I don’t really want to be bald if I can avoid it. So I started taking finasteride early on. However progesterone and finasteride both inhibit the 5-alpha reductase enzyme. And the finasteride, as it turns out affects a little more than just the 5AR enzyme.
Remember our little friend allopregnanolone from earlier? Blocked. What about isopregnanolone. Blocked. Finasteride is really quite a dirty drug with lots of off-target activity.
I’ve deemed it as unnecessary for the same reason I don’t take any testosterone blockers, such as cyproterone acetate or spironolactone. We’re going for estrogen dominance here. Women do have testosterone, but it isn’t the dominant sex hormone.
It is unclear if there is any added benefit to taking one of these medicines once your testosterone levels have been reduced into the female range through the use of other blockers.
The science behind it all is always a work in progress. But for now let’s keep that key phrase – estrogen dominance; the female hormone range, at the front of our minds.
If the presence of DHT makes male pattern baldness progress… what happens once I cease finasteride, will it also resume? Well, that’s where the next set of blood results come in.
Oh there it is, estrogen dominance achieved! Testosterone levels in AFAB have a reference range of less than 2.0 nmol/L (pre-menopause). And there I am sitting pretty at 1.1 nmol/L. My sex hormone binding globulin (SHBG) is heading up and up. I can’t find the document I had, I am sure it said above 115 nmol/L can result in estrogens being bound. In lieu of that article, from Wikipedia.
The relative binding affinity of various sex steroids for SHBG is dihydrotestosterone (DHT) > testosterone > androstenediol > estradiol > estrone. DHT binds to SHBG with about 5 times the affinity of testosterone and about 20 times the affinity of estradiol.
So having a high SHBG level is a good thing, the higher the better. Bind all the sex hormones so they can’t be used – male ones are lost first, then the female ones. That means goodbye any DHT generated by the mere 1.1 nmol/L of T.
The calculated free testosterone being below 25 pmol/L is also a great sign things are heading in the right direction. This is why testosterone blocking isn’t required for me. I really do enjoy delving into this sort of data and getting a better understanding of what it all means. So that’s it for now. I look forward to my next set of results sometime in May. 🙃